OK, this post is long, it's very long, but I've dotted it with lots of pictures to make it a bit easier to digest. The post has been a massive hurdle for me as I'd love to share more about Milo's day to day stuff on the blog but I feel like until I've got this published then I can't. Part of it is selfish therapy for my self and the other part of it is me rejoicing in how amazing my little boy is!
Whilst Milo's cardiac journey was traumatic, distressing and not straight forward it did have a happy ending. I'd love to hear how your journey's are going too?
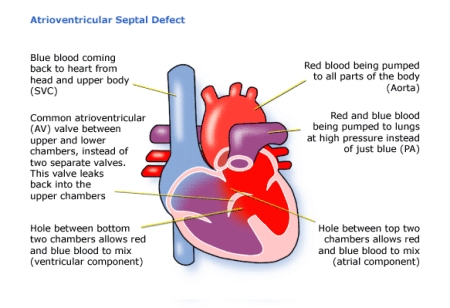
Milo had an antenatal diagnosis of a complete AVSD. At that time it wasn’t the devastating blow that most people experience as the prediction before this point had been that they had not expected him to survive the pregnancy due to a cystic hygroma and that he more than likely had the much more devastating condition hypolastic left heart syndrome. Because of this I think I had underestimated the impact that the heart condition would have both on Milo and us as a family.
Whilst Milo's cardiac journey was traumatic, distressing and not straight forward it did have a happy ending. I'd love to hear how your journey's are going too?
Milo had an antenatal diagnosis of a complete AVSD. At that time it wasn’t the devastating blow that most people experience as the prediction before this point had been that they had not expected him to survive the pregnancy due to a cystic hygroma and that he more than likely had the much more devastating condition hypolastic left heart syndrome. Because of this I think I had underestimated the impact that the heart condition would have both on Milo and us as a family.
He was induced and born weighing 2.84kg at 37 weeks without
any serious concerns. I had already
written in my birth preferences that I did not want him to be separated from me
and taken to the neonatal unit as a precaution but rather only if there were
clinical problems identified.
Milo did begin to struggle with feeding (Milo’s feeding
story to follow!) and jaundice and after a couple of weeks was readmitted with congestive
heart failure. We were surprised that he
was struggling so early with heart failure but were told that it was because as
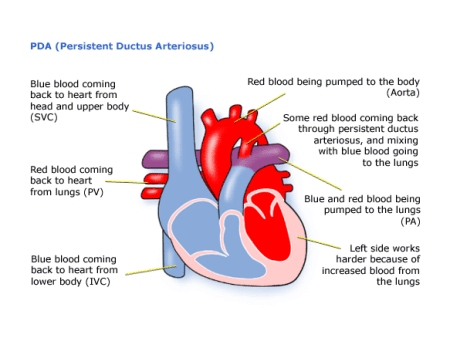
well as having a large complete AVSD he also had a large PDA which hadn’t
closed after birth in time this led on to pulmonary hypertension from too much blood being pumped to his lungs and flooding them.
Over the next month whilst in the hospital Milo was classed
as failure to thrive as we struggled to get the right balance of diuretics and
calories needed in order to help Milo to gain weight whilst preventing his
lungs from being overloaded with fluid. He worked really hard with his
breathing which was very fast and with chest recession and sweated an awful lot
with feeding.
By this point he was fully
naso gastric tube fed a high calorie combination of fortified expressed breast
milk and high energy formula although I also gave him daily practice at sucking
at the breast for 1 minute to help to maintain a sucking reflex. He was
discussed as a potential candidate for pulmonary artery banding (where they put
a band on the pulmonary artery to reduce the blood flow to the lungs to allow
the child time to grow). However despite
me pestering , by the time they’d got
round to discussing his case Milo was 5 weeks old and had finally started to
gain weight weighing 2.9kg so it was decided to hold out for a full repair
which we were told could happen when Milo reached 5kg. Milo was discharged from hospital on a very
complicated feeding regime but it wasn't to last.
Milo's daily breakfast
Within a few weeks he was readmitted struggling with his
heart failure and a nasty cold virus called RSV which causes bronchiolitis in
vulnerable babies. He was very poorly,
ghostly white from exhaustion and needed high dependency care with high flow
air/oxygen mix (optiflow) and further restricted fluids continuously fed
through a feed pump.
Poorly boy
It was a very
frustrating time seeing many other babies come in with similar symptoms only to
recover within 3-5 days. Milo took 4
weeks to recover and even then he was sent home on oxygen and no longer able to
tolerate bolus feeds due to him sweating too much and working too hard with his
breathing so instead needed a feed pump continuously.
Changing his face tapes has always been a trauma!
On the mend and first proper smiles for mama
He was only home for a few days over Christmas which was
really quite stressful being a 24hr carer for a very poorly baby and during
that time I was up and down to the hospital like a yo yo with various
concerns. His respiration rate was 80
and he was really struggling.
Then he
was readmitted with a very high fever which turned out to be influenza B. His oxygen saturations were dropping into the
40’s when he managed to sleep despite 6 litres of 100% oxygen via optiflow so
he was transferred to the children’s intensive care unit. It was a very scary
time.
The cardiologists liaised with the
doctors caring for him and they thought that he was probably having large
shunts of blood going through the holes in his heart. It was decided that as soon as he had
recovered from influenza that he needed his cardiac surgery as his heart simply
wasn’t coping. So after a few weeks of
another very slow recovery we eventually managed to get him off the optiflow and
said good bye to all the lovely nurse friends that had felt more like Milo’s
family since he’d been born and got into the ambulance for his transfer to
Alder Hey Children’s hospital.
Milo’s Sat’s were still dipping into the 60’s as he slept at this point and we had only managed to achieve a weight of 4.6kgs at 4 months old.
Very pale baby celebrating Christmas
 |
| Bruised head from repeated attempts at trying to get a line in somewhere, a central line was inserted in the end which was much easier to take blood gases from. |
Milo’s Sat’s were still dipping into the 60’s as he slept at this point and we had only managed to achieve a weight of 4.6kgs at 4 months old.
It’s worth noting that over the time of Milo’s heart failure
we had had 4 different oppinions from various experts over what were an
acceptable level of oxygen saturations for a baby with a complete AVSD and
PDA. 2 different cardiologists told us 89% and above, a respiratory expert told us that he should
have normal sats (above 94%!). In the
end his cardiologist who we’d transferred to told us that he would be happy
with sats of 80%! Although Milo was
still needing oxygen whilst he slept to even achieve this. I’d be curious to know what other parents experience of this piece of advice have been.
Arriving at Alder Hey was a very scary experience for
us. We had been used to our own private new
on-suite room at our local hospital where we knew every lovely nurse by name. Although here he was to stay on HDU and I was
told that I could not stay with him.
Thankfully a kind nurse allowed me to stay in a bed around the corner
from him although I didn’t get much sleep as I kept checking that he was ok.
I remember feeling that the build-up to his operation was so
intensely awful with me struggling to stay strong for my little boy having to
go through so many failed attempts at blood tests and agonising echo’s. I also wasn’t prepared for the bluntness of
the consent form and struggled to listen and stay focused after they stated the
10% risk of mortality figure due to his oxygen dependency, pulmonary
hypertension and size. We were aware
that the reason that they’d held off for so long in performing his surgery
whilst he struggled with heart failure was because of the difficulties in
making the new valves that are needed when an AVSD is complete. The surgeon informed us that the difference
of an extra month can mean the difference between the valves being as thin as
paper, clear and soft as butter to something much tougher that could hold the
stitches in place. Although they agreed
that Milo could not wait any longer for his surgery.
We were told that he would probably have his operation the
next day but I didn’t like the uncertainty and told them that I’d rather he
wait an extra day than compete with 2 other patients and for them all to be
starved when only 2 could go to theatre.
My concerns were brushed over though as they needed to get as many children
through surgery as possible and if there was a chance of getting 3 done then
they’d rather starve 3.
The next morning we were up early to give Milo his last bit
of milk and wipe him down and gown him up.
I took lots of photos of him smiling and playing with daddy in the dim
light of the ward frightened that they may be the last ones that I’d get of
him. After many hours of waiting for
news we overheard the doctors casually mention to a nurse that Milo wasn’t for
theatre today. I felt so cross as I’d
predicted that this would happen and although Milo didn’t necessarily feel
hunger due to being continuously tube fed for so long I wanted to make the
experience a smoother ride for all of us as it was already so stressful. The day didn’t get better as Milo was
accidentally given aspirin off another child’s drug chart despite my husband’s
protests that he wasn't on aspirin. The
nurse admitted to us later that she had made a mistake and was deeply sorry. Although disturbed by this error the nurse
had shown genuine empathy that day and we wanted to move on. Surgery was scheduled for the next day and
the surgeon was happy to still proceed despite the error.
Sitting down to go through the detailed consent form with
his surgeon I remember staring at his long slender fingers and neatly trimmed
nails praying that these would be the hands that in his words would ‘prolong
life’
.
.
The following morning we once again went through the ritual
of the dozens of ‘last’ photos and cuddles with our heart in our throats.
Milo was 1st on the list and so at 8.45 am I carried him into the anaesthetic room and lay him down on the heated squishy mat on the bed, gently kissing his head as he breathed in and licked the gas mask. Walking back along the corridor to his dad I cuddled Milo’s puppy before hugging Adam. We went back to our room and did our best to keep busy, do washing, tidy up. All the time thinking of what was possibly happening to my little boy at that moment. We’d been asked not to leave the hospital grounds in case they needed to speak to us urgently or ask for us to consent to further urgent treatment.
Milo was 1st on the list and so at 8.45 am I carried him into the anaesthetic room and lay him down on the heated squishy mat on the bed, gently kissing his head as he breathed in and licked the gas mask. Walking back along the corridor to his dad I cuddled Milo’s puppy before hugging Adam. We went back to our room and did our best to keep busy, do washing, tidy up. All the time thinking of what was possibly happening to my little boy at that moment. We’d been asked not to leave the hospital grounds in case they needed to speak to us urgently or ask for us to consent to further urgent treatment.
I tried to relax and take a bath, but as soon as I got in
the bath my phone rang from an unkown caller. ‘It’s one of the nurses on the
ward we’re just wondering if you could come over to speak to the consultant as
he needs consent’. I almost had a heart
attack as I was stuttering to ask her what for , splashing water everywhere as
I dived out of the bath. She then
explained that it was consent for his gastrostomy tube that he would have
fitted the next day. I was so cross that
they’d rang about that at this time yet so relieved that it was nothing serious.
After consenting for the gastrostomy tube I was impatient
and couldn't bear to wait in the Ronald Macdonald guest house. So instead we spent the last couple of hours
of Milo’s op in the intensive care unit waiting room. All I needed to know at that time was that
he’d made it out of theatre ok. I couldn’t bear the thought of him being in ICU
without me knowing. It was therapeutic
to start to speak to other parents about their experiences whilst I was
waiting. The last hour dragged and I
spent it mainly in the corridor outside of the ICU doors, desperate to get a
glimpse of his cot and entourage being wheeled behind the door.
The relief when I saw him was incredible and after 25 minutes of badgering staff they finally allowed us in to sit at his bedside. They were great at explaining what everything meant, every tube, wire, mark on him. Within minutes though Milo was writhing and wriggling all over the bed, kicking his legs out. I was anxious that this wasn’t supposed to be how he should be, minutes after surgery. Then his surgeon came and discussed with the nurses that he wanted Milo ‘flat’ for the next 24 hours to allow his heart chance to rest. He explained that the operation had been complicated and tricky but that he was happy with the repair. He said that his heart was ‘massive’ and his pulmonary hypertension very high.
We felt unbelievably relieved to be the other side of his surgery although we were anxious that the next 48 hours at least would be critical.
The relief when I saw him was incredible and after 25 minutes of badgering staff they finally allowed us in to sit at his bedside. They were great at explaining what everything meant, every tube, wire, mark on him. Within minutes though Milo was writhing and wriggling all over the bed, kicking his legs out. I was anxious that this wasn’t supposed to be how he should be, minutes after surgery. Then his surgeon came and discussed with the nurses that he wanted Milo ‘flat’ for the next 24 hours to allow his heart chance to rest. He explained that the operation had been complicated and tricky but that he was happy with the repair. He said that his heart was ‘massive’ and his pulmonary hypertension very high.
We felt unbelievably relieved to be the other side of his surgery although we were anxious that the next 48 hours at least would be critical.
Well Milo needed longer to recover than 24hours and for the
next few days we battled with Milo’s bleeding requiring transfusions and extra
stitches, fast heart rate and high temperature as well as sedation, blood
pressure and swelling issues. They
dressed him in a cooling jacket in an attempt to bring his temperature down and encourage more fluid back into his circulation and prevent his blood pressure from dropping so dangerously low.
At 1 point I as I was discussing with the doctors that I was concerned that he might be feeling pain his heart started losing all out put function. Within seconds a curtain had been dragged across as staff rushed to his bedside and someone carried the emergency drug box. Thankfully with early intervention and an extra shot of adrenaline they managed to stabilise his heart again although they were still concerned about how much fluid he had collected as he was grossly swollen.
At 1 point I as I was discussing with the doctors that I was concerned that he might be feeling pain his heart started losing all out put function. Within seconds a curtain had been dragged across as staff rushed to his bedside and someone carried the emergency drug box. Thankfully with early intervention and an extra shot of adrenaline they managed to stabilise his heart again although they were still concerned about how much fluid he had collected as he was grossly swollen.
Every time that I would leave him to get a drink or make a
call I felt sick to my stomach not knowing what the new drama would be that I
would return to. I hated leaving him at
night and would spend time ensuring that I got to know his new night nurse
before I entrusted him in her care. I
always wanted to show them a photo of who the real Milo was as I was aware that
he just looked like a body to them and I
wanted them to feel what a special little boy he was that they were caring for.
When I got up at 2 am every morning I would ring to ask how he was, but luckily
most of his dramas seemed to unfold during the day. Returning at around 7am each morning meant
that I’d get to hear the full hand over of care to his new nurse ensuring that
I regained a tiny bit of control over a situation in which I felt
helpless.
Milo was really really swollen his eye lids didn’t close and
the membrane on his eye was also swollen and bloodied. 4 days had passed since
his surgery and he’d remained ventilated the whole time as he’d been so
unstable. The fluid had taken advantage of the empty pocket of skin around his neck where he'd had a cystic hygroma when I was pregnant, he was so swollen that his head molded to a wedge shape and he had to be rotated regularly to help to shift the fluid around his head. But after 5 days there was talk that we were going to try to extubate him and get him breathing by himself.
.His dad left the hospital as he had to return to work the next day. From this point on I was on my own.
The next morning though Milo wasn’t happy, I didn’t feel as
though his pain relief had been kept on top of as he’d just had paracetamol,
the ICU was shut down and I was asked to leave. An hour later I was urged to return
before the other parents as the staff couldn’t seem to soothe Milo’s constant mews of
discomfort. His skin was mottled and his
legs and arms turned a deep shade of purple.
A blood gas confirmed that he was struggling too much. For half an hour I held his tiny hand as they
tried to help him using a mask and positive airways pressure (CPAP) but his
blood gas was still awful so they decided to reintubate him and I was forced to
leave his side for the procedure once again.
His tummy looked a bit swollen and I wondered if he’d had tummy ache and if we’d pushed him too far with the bolus feeds too soon.
His tummy looked a bit swollen and I wondered if he’d had tummy ache and if we’d pushed him too far with the bolus feeds too soon.
On returning the echo showed that his valves had started to
leak too much but the doctors thought that if they gave him a bit more time to
lose some of the fluid that he’d been storing then his heart wouldn’t have to
work as hard. Then his stomach started
to swell more and more and after a couple of days it was huge and shiny and
there was a dark patch on the surface where the tissue had begun to die.
His liver was also clearly visible below the
surface of his skin, floating and massive, a clear sign of severe heart
failure. I broke down at this stage
fearful that it was obvious to everyone else that he was dying and they didn’t
want to discuss it. A quote from the Heart
Line children book stuck in my mind which said ‘Although parents may suspect
that their child is dying, they may be afraid to ask and have their fears
confirmed. Hospital staff tend to focus
on the positive and may avoid voicing concerns that a child is deteriorating’. The staff tried to reassure me that they were
doing everything that they could for Milo. It was thought that Milo had necrotising enterocolitis, a very serious gut infection,
so we rested his gut from feeds and put him on TPN (nutrition through the vein) and also removed his groin arterial line in an
attempt to improve his circulation to his tummy and legs. Green faeces started to emerge from his NG tube
and my baby felt no longer recognisable.
How could we come back from this point?
I was exhausted from the constant worry and the fact that I felt that I had to be on the ball all of the time as I was the only person who had had full continuity with Milo throughout all of his difficulties. But again he started to improve, his fluid decreased and after another few days they felt he was ready for extubation.
I was exhausted from the constant worry and the fact that I felt that I had to be on the ball all of the time as I was the only person who had had full continuity with Milo throughout all of his difficulties. But again he started to improve, his fluid decreased and after another few days they felt he was ready for extubation.
They weaned his sedation so that I had ‘my Milo’ back with me
but he was panicking that he had tubes stuck in him everywhere. At the time one of the lovely nurses from our local hospital had been so kind to come and visit Milo to see how he was doing, everyone there was also worried about him. He started to work harder with his breathing
and ‘fight’ the vent. The doctors wanted
to give him another hour or so before removing the tube to see how he did. But stuck in this limbo was like torture for
him and soon his arms and legs were cycling wildly whilst his eyes were wide
and staring intently at me in panic whilst I struggled to hold his hands to
calm him down. Then I heard the bubbling
and saw that his breathing tube (ET tube) was full with blood. They suctioned him but it kept coming’ more
and more. They quickly sedated and
paralysed him again to stop his gag reflex from all of the blood and make him
more comfortable. I grasped Milo's visiting nurses hand as we watched them work on trying to stabilize him. A massive pulmonary haemorrhage
was confirmed via X ray, as the image showed his lungs were completely white and
filled with blood. He had been drowning
and I’d been pinning him down. I still
feel traumatised by this event today. He was fully sedated again and I was relieved that he was getting some
relief from this torture. They had to
turn up the ventilation to its maximum to try and stem the bleeding and he was
very close to needing oscillation (higher frequency ventilation for difficult
to ventilate patients). He was given
blood transfusions, vitamin k and fresh frozen plasma, all in an attempt to
stem the bleeding. I remember googling
what the haemorrhage meant only to see my screen filled with the word fatal, I
knew it was serious. I rang my husband
and asked him to come be by my side as I didn’t know what would happen.
The next morning the consultants broke it to me that Milo
was very poorly. That they suspected
that he’d got endocarditis. Previous tests that I had not been made aware of were showing that his lungs were positive for pseudomonas
and ecoli and that they didn't think that they would be able to get him off the
ventilator with such bad regurgitation of his heart valves. Furthermore, that if he managed to recover
from this infection that the only option would be to take him back for more
open heart surgery and attempt to repair his valves. Only he was so small that they didn't know
how they would be able to repair the valves, as he suspected that the sutures had torn through his valve tissue
which is as thin as paper but clear. He
was too small for transplants or mechanical valves too. I hit rock bottom that day, I started going through the grieving process sobbing
and wailing, furious at staff for missing things or not keeping me informed
before this point about the possibility of infection. Denial that this couldn't possibly be happening to me, bargaining that they must of missed something, that they had to do something. Until this point I’d asked
for visitors not to come to ICU but to wait until he made it to the ward but I
sent the text out asking them to visit him and telling them that the outlook
wasn’t optimistic. The unit was shut down as a child needed an emergency
operation in ICU but I was sobbing so much that they let me stay with my
precious boy, stroking his head and singing him songs.
At my lowest point that day (and I’m really opening my heart
up now) I was having the daily battle that Milo’s sedation wasn’t enough, that
he was distressed and in hysterics I thought that I wanted someone to end it
for both of us now. I thought that it was utter torture for him and torturous
for me to have to stand by and watch my baby suffer for so long. I even questioned whether I’d done the right
thing in not terminating him and bringing him into a life of pain and
suffering. In retrospect now I think
that these thoughts were a reflection of how traumatic I found the experience. I know that the experience has had absolutely
no lasting effect on my amazing happy boy, on the contrary it has given him the
gift of life. In writing these thoughts
down now I'm doing so not to wallow in self pity but to process and help myself overcome the lasting emotional distress of the situation whilst sharing with parents that these feelings of despair are normal in
this sort of situation
.
Sitting in cubicle 2 and watching the 10th child
come and go back to the ward following their open heart surgery was also
equally hard. I sobbed when I expressed
him milk wondering why I was doing it and what I’d do if I lost him. I went back to ‘Mac house’ that night and breathed in his baby grow that
he’d worn before he’d gone to theatre, too scared to wash away his smell. The next morning I found myself saying ‘if’
he survived to a member of staff and then I realised that I couldn't function
like this. I decided that this was too
unbearable and that I had to stay strong and be positive for Milo, to help both
of us. I decided to focus all of my
energy on ensuring that he had adequate sedation and pain relief at all times (we
could deal with withdrawal at a later stage) and that I was fully up to date
with all of his test results. I had to
help Milo and he HAD to get through this.
So they pumped him with antibiotics in a desperate
attempt to save him whilst they rested him.
I remember looking at his
terribly pale and bloated pin cushion of a body struggling to even remember
that it belonged to ‘my Milo’ . Then they were having issues with his blood
pressure again, and his raised temperature.
At this time, people all over the
world were supporting us and thinking and praying for Milo. We were inundated with get well soon messages
and messages of support, it was so lovely and really helped to keep my spirits
up.
ry.
After many days and a false hope of it happening on the Monday they finally decided that Milo was as strong as he was ever going to be to return to theatre for further open heart surgery on the Thursday. His heart was having strange arrhythmias called ‘bi-geminy’ and SVT and we were told that we should expect Milo to be very poorly if he made it through his operation. We were informed that the risk of fatality from this 2nd operation was double that of the first operation and that it would take longer. He would more than likely need Ecmo (a form of long term bypass) to give his heart chance to rest and recover following surgery. They also arranged for lots of extra skilled members of the surgical theatre team to be present during his surgery in case of complications.
ry.
After many days and a false hope of it happening on the Monday they finally decided that Milo was as strong as he was ever going to be to return to theatre for further open heart surgery on the Thursday. His heart was having strange arrhythmias called ‘bi-geminy’ and SVT and we were told that we should expect Milo to be very poorly if he made it through his operation. We were informed that the risk of fatality from this 2nd operation was double that of the first operation and that it would take longer. He would more than likely need Ecmo (a form of long term bypass) to give his heart chance to rest and recover following surgery. They also arranged for lots of extra skilled members of the surgical theatre team to be present during his surgery in case of complications.
On the day of his surgery we got hand and foot prints from
our beautiful baby and kissed him goodbye once again. Then we headed back to
our room in Mac house where we tried but failed to think about anything but his
surgery. An amazing parcel of gifts had
arrived on ICU just minutes before he’d gone to theatre. It was from the lovely members of The Future
of Downs forum who I’d had fantastic support from and it was an really uplifting gift which arrived just at the right time. Then,
after less time than expected, we got the phone call from Milo’s lovely nurse
Amanda to say that he’d made it through surgery and was back on ICU. We couldn't believe it and practically ran
across the road to see him. He was
looking good and Amanda was also amazed that he didn't have any complications
at that time.
The surgeon came to explain what he’d found and said that
Milo’s heart was mushy inside as though he’d had early stages of
endocarditis. He said that his valve
looked as though it had exploded from underneath although the original sutures
were still in place. He had managed to
patch his valve up with a piece of bovine pericardium and whilst the repair
wasn't perfect it was working and Milo had tolerated the operation well. They were much more cautious with Milo’s
recovery after this 2nd operation, but he surprised everyone and did really well. They spent longer ensuring that his swelling
significantly reduced. 3 days later they
were going to attempt extubation when they realised he wasn’t tolerating it. Unfortunately
he had to have another chest drain in which revealed a chylothorax (leakage of
lymphatic fluid into the pleural cavity).
The following day he was ready for extubation and although I had a
moment of tearful panic remembering the previous attempts I was relieved
that it all went smoothly. I finally got my
first tentative cuddle in 3 weeks, oh how amazingly fulfilling that felt. Finally my 3 week bedside vigil on ICU came to an end as we headed for the ward.
The next day he was back on the ward where he spent another
long 3 weeks. At first it was hard to
adjust to the fact that he didn’t have a 1-1 nurse but as he got better and was
moved off of the HDU bay we were given a side room and I was finally able to
stay overnight with my baby and relax a little in each other’s company. We tried for a week getting Milo’s
chylothorax leakage to reduce without altering his diet (breast milk, but now
not fortified) but after 7 days the leakage was still around 50mls per day and
so the team decided it was best that we try to swap Milo’s milk to
Monogen. Well that didn’t go down well
at all. Milo persistently vomited, had
green thick mucousy stools and became dehydrated and tachycardic. Enough was
enough so we put him back on to breast milk and he got better, but the chyle
took another 10 days to reduce back down to 40 mls per day before they decided
that they could remove the drain. I was pleased that the hospital had worked flexibly
with me over the chylothorax and changing of his diet. In most hospitals it would
be unheard of for children not to be changed to Monogen milk straight away, despite
there being no evidence to support this intervention. Within 24 hours of them removing his drain we
were finally home after 6 weeks in Alder Hey and many months being in hospital, it was like bringing my new baby home from the hospital all over again.
Milo was kept on diuretics for a few weeks and has been on
long term lisinopril but is doing well although we never stop worrying about
him and his heart. We've been told that there is a 30% chance that he'll need his valves replacing as he grows (although 1 cardiologist told us that he would certainly need them replacing before he's 5). We're always on the look out for symptoms of heart failure returning with him. He’s continued to
struggle a little with his respiratory issues and needed oxygen at home for a
while but this seems better during the summer so we’re keeping our fingers
crossed for a better winter too!
I suppose I wanted to share Milo’s cardiac journey as it is
a testament to everything that he has overcome.
He truly is a little fighter. I
also want to give thanks to the amazing cardiac surgeons and their teams
without them many lives would be lost .
We’re planning on a big 1st Birthday party for
Milo where we hope to raise funds for the hospitals where Milo was cared for. Although it will be an emotional day we can’t
wait to celebrate it!


































No comments:
Post a Comment